Looking Into Breast Imaging
Videos
Looking Into Breast Imaging Part One
Looking Into Breast Imaging Part Two
Audio
Radiologist Sue Jane Grosso-Rivas, MD, joins cardiologist and clinical researcher Michael J. Koren, MD, to share her inspiring journey from aspiring secretary to Medical Co-Director of Breast Imaging at Summit Health. The doctoral duo discuss how Dr. Grosso-Rivas’s career was shaped by a school counselor who recognized her potential and encouraged her ambition.
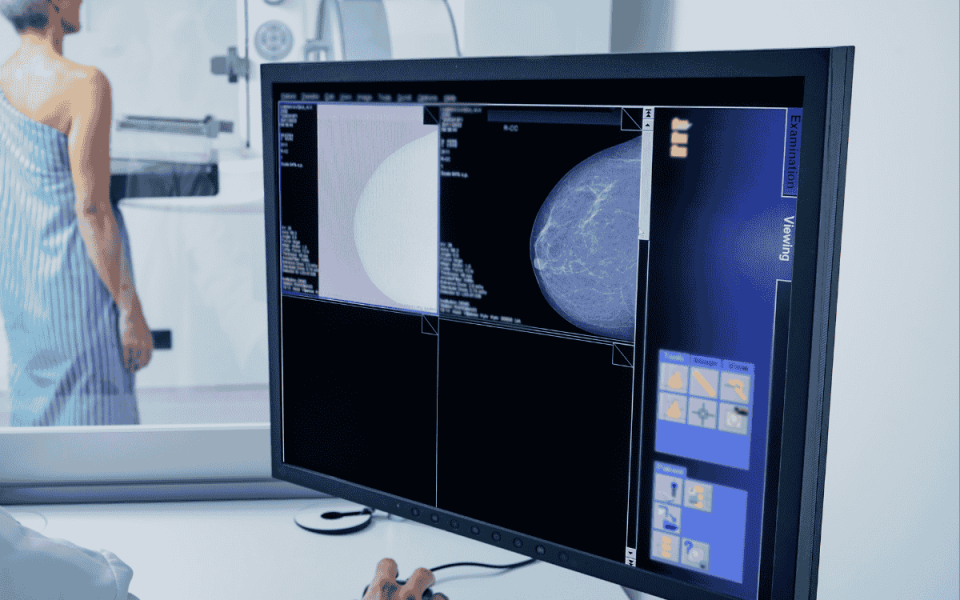
Dr. Grosso-Rivas explains the fundamentals of breast mammography, including when patients should begin screening and how to ensure high-quality care for breast cancer prevention. She then explores what happens if mammography finds an abnormality, including whether it is benign, suspicious, or indicative of cancer.
In Part Two, Dr. Grosso-Rivas talks about some of the complications that can occur during imaging, including dense breasts and their surprising prevalence. She also talks about new technologies in the imaging world, including contrast mammography and the use of AI in cancer detection. She finishes the conversation by talking about men's mammography and the increase in young-onset breast cancer in some populations.
Transcripts
Transcript Generated by AI.
Announcer: 0:00
Welcome to MedEvidence, where we help you navigate the Truth behind medical research with unbiased, evidence-proven facts Hosted by cardiologist and top medical researcher, Dr. Michael Koren.
Dr. Michael Koren: 0:11
Hello, I'm Dr. Michael Koren, the executive editor of MedEvidence! And I have a really, really special guest today who is part of our Master Series, where we take the best and the brightest and we have those people break down their area of medical expertise and share that with our listeners and viewers and break it down from the standpoint of a patient's journey. And today I'm delighted to introduce Sue Jane Grosso-R ivas, who is an expert on breast imaging and her current position is a breast imaging director for Summit Health. But also lots of other wonderful things on your resume in terms of advising the FDA on accrediting breast imaging organizations, and I think, if I remember correctly, you also have a role as an expert with the American College of Radiology. So you can break that all down for us, Sue Jane. But welcome to MedEvidence! Thank you so much for being part of this podcast.
Dr. Sue Jane Grosso: 1:11
Thanks, Mike. I'm very happy to be here and happy to share whatever information I can to enlighten everyone about breast imaging. Absolutely, thank you.
Dr. Michael Koren: 1:21
So Sue Jane and I had a really interesting interaction actually at our reunion from Harvard Medical School and I won't say what number reunion it is, because I want to protect the innocent from identity theft and age discrimination.
Dr. Sue Jane Grosso: 1:35
Very glad to hear that Most people don't know my age, Mike.
Dr. Michael Koren: 1:41
Well.
Dr. Michael Koren: 1:42
I wouldn't know your age, except for the fact that we went to medical school together.
Dr. Sue Jane Grosso: 1:51
That's right. I started very early.
Dr. Michael Koren: 1:52
There we go. Yeah, that's a good thing to tell people. I love that, but anyhow. So you shared a super interesting story about how you built the confidence to actually go into medicine and ultimately apply to Harvard, and it was interesting to me because we both have the commonality of having grown up in New York City and having experiences there, and so I'll let you get to that in a second. But it was a fascinating journey and was part of the reunion, which is my favorite part of the reunion, where all of our classmates just kind of share their stories. And one of the wonderful things about getting older is that you get very comfortable with yourself. You use the term, you feel good in your own skin and you're less worried about what people think and more worried about sharing your experiences and maybe helping other people by virtue of the sharing of those experiences.
Dr. Sue Jane Grosso: 2:37
Absolutely.
Dr. Michael Koren: 2:38
Yeah.
Dr. Michael Koren: 2:39
So tell us a little bit about how you grew up and sort of repeat the story that you shared with our classmates.
Dr. Sue Jane Grosso: 2:53
Well, Mike, you know, when I wrote my report for the reunion, I decided that I wanted to share my story and tell what I considered the truth of who I was. I feel that a lot of times, people you know don't, just by looking at me, you can't. You know, you can't tell right, you can't judge the book by its cover, you have no idea where they've been basically, and I thought that it would be a story that maybe would motivate others or inspire others, and so I did want to tell the story and I titled my story If you remember, it was called East Side Story.
Dr. Michael Koren: 3:21
Yeah, I love that.
Dr. Sue Jane Grosso: 3:22
And the reason it was because I my favorite musical was West Side Story and it was because I felt that it kind of told my story. Because my mother was from Puerto Rico. She came to United States at about the age of 18. And my father was a first generation Italian American. My grandfather came from Italy and settled in the South Bronx. So my mother, being the, you know, the Puerto Rican from, let's say, West Side Story, and my father, who was Italian, not Polish as Tony, was in West Side Story, but you know the fact that their union was was not a common one back in the 1950s and in fact it was a beautiful love story, certainly, but my mother was not accepted by his side of the family and so, unfortunately, it led to them breaking up. They were separated and I ended up raised by my mother alone.
Dr. Sue Jane Grosso: 4:22
So it was a single parent household which then changed a lot of things for me and it was, you know, living in a lower income neighborhood, basically, and I was going to a school in East New York and it was at a time when they started to bus students. It was part of the desegregating program. I don't know if you remember from that time they were trying to create equality in education by taking students from a lower income neighborhood and bringing them into another neighborhood. So I was bused from the east side of Brooklyn to the west side of Brooklyn and that was Bensonhurst. So I ended up in Bensonhurst where there was a better educational opportunity for me. I ended up in. It was elementary school. I started at fifth grade, but I remained there, even though I moved. You know, in Brooklyn my family moved to several different parts. I continued to travel to Bensonhurst and I ended up at a high school, New Utrecht High School. That was a great public high school. They had honor classes. So there were other students that were interested in learning, like I was, which is very important to be surrounded by people that are similar as far as their goals.
Dr. Sue Jane Grosso: 5:40
But, as you remember, the story was that what really changed things for me was when I went to my high school counselor, Sylvia June Goldberg, and I'll never forget her. I went there and you know, as many counselors sometimes do, right, not all of them are great, but this particular counselor asked me what I wanted to be and I said a secretary. And she looked at me and she said a secretary, and I said, yeah, a really good secretary. I'm going to be a bilingual secretary. I'm going to be an executive secretary, I'm going to be the best secretary there is. And, by the way, I did take typing and I was very good at typing and very fast, and that's one of the best classes I've ever taken.
Dr. Sue Jane Grosso: 6:22
So, anyway, but she looked at me and she gave me the lecture that would change everything. She started out telling me that I could be anything I wanted to be, and she described that there was a ladder that would reach to the sky and I should climb this ladder to the top and if, for some reason, I couldn't get to the top, it was okay to come down one rung right. She said I could be anything. I could be a doctor, I could be a lawyer. And it just opened up my eyes to something I never really thought about.
Dr. Sue Jane Grosso: 6:56
You know, I was very good in science, I was very smart, there was no doubt about that.
Dr. Sue Jane Grosso: 7:00
I was excellent in the sciences, excellent in math, and so I thought, okay, so I guess I could be a doctor. And then I said, well, what about a nurse? I could be a nurse too. And she looked at me and said well, let me ask you this question Do you want to tell people what to do, or do you want them to tell you what to do? And I thought, oh, I want to tell people what to do. And to think that at that age I don't know, maybe I was 13, 14 years old, 15, I don't remember, but it was so clear to me. And I went home that day to, my mother was in the kitchen cooking some fabulous Puerto Rican meal and I looked at her and I said, mommy, I'm going to be a doctor. And she looked at me. She goes okay, but never expected, never expected that I would reach those heights. But it was all because of Sylvia June Goldberg. She really, she really started me on that path.
Dr. Michael Koren: 7:56
Well, that's fabulous and we take our hat off to her. Is she still with us? Is she still alive?
Dr. Sue Jane Grosso: 8:02
No, unfortunately she is not. I have looked her up and I feel badly that I didn't get to speak to her to thank her. And I even looked her up to see if maybe she had children or there was someone that I could connect with, but I have not been able to find that. I don't think she had children. I didn't find that information, so it's unfortunate. I did try reaching other teachers that I did.
Dr. Michael Koren: 8:27
I'm glad that you're able to give her a tribute. That's fabulous. I will say that clearly. She was an inspiration to you and, I'm sure, to many other students. But she may not have understood medicine exactly, because in my experience the nurses tell the doctors what to do.
Dr. Sue Jane Grosso: 8:42
Quite right. I mean, look, nurses extremely important. Love all of my nurses for sure. But ultimately, you know, as a physician, you do have to end up making a lot of the decisions. So you know people, even with what I do today, as they say, the buck stops with me. It's like they expect me to make the decision for anything that's going on with a particular patient.
Dr. Michael Koren: 9:07
Yeah, absolutely, of course. So tell us a little about your journey from graduating medical school to your training. How'd you end up getting involved in breast imaging, what was, where were the inspirations there and how you eventually got to where you are now, which is you which is leading a big group at Summit Health, and, along the way, you can mention that we have a number of commonalities. You probably don't know this, but I was actually born in the Bronx.
Dr. Michael Koren: 9:33
I was born at Bronx Lebanon Hospital and I grew up on Staten Island, where I know that you spend some time, so maybe share with us in the audience exactly how your path played itself out.
Dr. Sue Jane Grosso: 9:47
Well, you know, as you remember, Mike, when we were at Harvard Medical School, you know, when you are in medical school, you get to do many different rotations as you're trying to figure out what kind of a doctor you will be. When we were at Harvard, if you remember, they really pushed primary care. Do you remember that Primary care was something that was valued very much and I thought I would be a primary care physician, a family physician. I knew that I loved taking care of people. I knew that. I knew that I wanted to probably be a primary care doctor.
Dr. Sue Jane Grosso: 10:19
However, as I went through my rotations one of the rotations that I went into, and I'll tell you I really enjoyed all of my rotations every single specialty that I went through, I would go. I don't know if that happened to you, but I'd go to psychiatry, do something in psychiatry. I think, oh my God, this is great, I could be a psychiatrist, or I, you know, do OB, you know OB. And next thing, you know, I want to deliver babies. So everything excited me, including surgery. When I did it at Mass General, I thought, oh my God, I have to be a surgeon. But when I did radiology at Mass General Hospital I don't know where you did your rotation, but it was Dr. Navaline who was in charge of the program.
Dr. Michael Koren: 10:59
I did it there as well.
Dr. Sue Jane Grosso: 11:02
Did you do that one?
Dr. Michael Koren: 11:02
I did radiology and surgery at Mass General, yeah.
Dr. Sue Jane Grosso: 11:04
Okay, I did both also at Mass General, but it was so well organized and I don't know if you remember when they put us into a room to sit down and look at cases, right. So there were these folders. They were called the American College of Radiology folders of images and I know this may sound corny and it may not. It doesn't even sound like it's possible. However, I reached into a folder, I pulled out an image and I put it up onto the view box, which is what radiology does, and I tell you that it clicked for me. I looked at that image and I felt like it was comfortable. It felt like like this is something I wanted to do. Then, looking back, I realized well, when I was in high school, I did take a course in photography, I was very interested in art, I loved anatomy and I think that looking at an image right was all about. It was black and white, so that was photography, and then you had to go through a differential and you had to kind of figure out what was going on based on that image. So for me, I found that very exciting. I thought this is and not only that, with radiology, it involved all specialties right. So it involved orthopedics, gynecology, oncology it was all there for you in radiology.
Dr. Sue Jane Grosso: 12:36
However, I will say that once I started my radiology residency, which was at New York University, I didn't realize that radiologists some of them do not have much of an interaction with patients. If you've heard, radiologists are people that those are doctors that don't want to see patients, they don't want to interact with patients, and that was not me at all. So when I was doing my radiology rotation at NYU is when mammography was just starting to get to to to be popular. There was no fellowship in mammography at that time and I met a professor that was brought in to NYU to head up the breast imaging department and that was where I found my patient connection again, because in in breast imaging we talk to the patients when they come back with something abnormal on the mammogram. We see the patients, we interact with the patients and I also do biopsies. So it sort of gave me the opportunity. You know how I wanted to do procedures when I saw it in surgery. So it gave me a little bit of everything.
Dr. Sue Jane Grosso: 13:45
And not only that with um, with breast imaging. I was also able to do, uh, some work in the community. So a lot of public speaking, and I wanted to help women. I became clear I wanted to help women and so I wanted to go into breast imaging and I knew that I could help them not just individually, but being a radiologist with a specialty in breast imaging meant that I could get on that bandwagon where everyone was talking about screening mammography and how it was so important. How do you get that message out to people? So I did a lot of work out in the community, whether it was radio, tv, public speaking, just trying to bring the word out to everyone about screening mammography. Until this day, I still do that, which is, you know, describing the latest technology, whatever it is, to go out and educate the people. So for me it was a perfect fit. I felt like I had found exactly what maybe I was meant to do.
Dr. Michael Koren: 14:41
Beautiful. I love that I love that. It's different for me. Yes, another, you just triggered our memory. I remember during our Mass General Radiology Clerkship, Lucy Squire was the leader who was a female during a time period there were a few physician leaders who were female who basically had set up the entire course and the training at one point. I don't know if that was an inspiration at all, but it was something I remember and to me was kind of neat to see that.
Dr. Sue Jane Grosso: 15:11
Yeah, no, it's true. Actually, when I went to NYU they only allow maybe one woman per year. Actually there were eight residents. There was one woman my particular year they happened to have they did take two women. But even back then I mean radiology and even the practice that I joined. Eventually, I mean, I did go to Staten Island and I guess I should digress, go back to how I ended up at Staten Island. But when I eventually ended up in New Jersey, I was part of a group, a private practice group, and they were predominantly all men. I was the second woman to join in 2001. So nowadays there are a lot more women in radiology.
Dr. Sue Jane Grosso: 15:50
But Staten Island, how did I end up in Staten Island? Well, when I graduated NYU, I actually went to California for a little while. I was there for about a year and a half. I joined a group that had connections with University of UCSF and also Stanford. So a lot of the radiologists came from those groups and I was there and I wanted to do breast imaging as a specialty and also nuclear medicine, because I did both of those but they weren't ready for what I wanted to do.
Dr. Sue Jane Grosso: 16:20
And in Staten Island, staten Island University Hospital.
Dr. Sue Jane Grosso: 16:24
The person that was in charge of the radiology program was a woman and she was at the cutting edge of where breast imaging was at that time and she created a little women's imaging center with all new mammography machines and at that time nobody was doing breast biopsies on Staten Island.
Dr. Sue Jane Grosso: 16:42
I'm talking about the not the breast biopsies in the operating room, but the minimally invasive breast biopsies that are image guided. So she brought me in to create that program, which meant that I had to go up against surgeons right, because surgeons were used to taking patients to the operating room for any biopsy, many of them which were benign. So I had to start up that program, start up a screening program, and so that was very exciting. That's how I ended up at Staten Island University Hospital. I was there for about eight years until I had an opportunity, you know, to come and join a private practice. Again joined the private practice only because it was an opportunity to start a program that they didn't have before. So I was always looking for leadership positions, something where I could make a difference and create a change that was ultimately helping the individual woman but also helping the entire community.
Dr. Michael Koren: 17:34
Yeah, absolutely. So we definitely both share the Staten Island parts of our story and the desire to make a difference. I think that's. It's a characteristic that some people in medicine have and others don't, and clearly you have that. So, one of the reasons I was so impressed by your little, speech at the time of our reunion.
Dr. Michael Koren: 17:47
But let's transition a little bit and talk about the patient journey. Obviously when you talk about breast imaging you talk about lots of people, obviously half, actually over half of the
Dr. Michael Koren: 18:09
American population and maybe even some men you can throw into that mix as well as I'm sure we'll get to that, but you talk about something that creates a lot of concern, anxiety and, ultimately, something that is incredibly important in terms of the early diagnosis of breast cancer and hoping to minimize the impact of that disease. So kind of walk us through a little bit about general recommendations for women and then we can talk a little bit more about people who are at higher risk and how you might tailor the strategies for those folks.
Dr. Sue Jane Grosso: 18:41
Well, you know, I think let's start at the beginning. As far as breast health, right, how do we maintain breast health? And, at one time, and you may remember this, the American Cancer Society, right, which is one of those societies that we look to to help us figure out when to get your mammogram. You know screening, and do you remember when they would talk about breast examination, self-examination?
Dr. Michael Koren: 19:05
Self-exams.
Dr. Michael Koren: 19:06
Yeah, there was a huge emphasis
Dr. Sue Jane Grosso: 19:08
And it was a big push, for this is how you do a self-examination, and so forth. So when they were talking about how to find breast cancer, they would say get your mammogram. And they would say examine your breasts. Right, this is the way you do it. Go into the shower, so on and so forth. I don't know if you know this, but they no longer recommend that you do breast self-examination.
Dr. Michael Koren: 19:30
Interesting.
Dr. Michael Koren: 19:34
Yeah, I haven't heard that lately and that makes complete sense, but you're absolutely right.
Dr. Michael Koren: 19:37
It was a huge point of emphasis about how to do self-exams and what time of menstrual cycle you do it and all that sort of thing.
Dr. Sue Jane Grosso: 19:44
Right, exactly, but they don't recommend it anymore. But I'm going to tell you that, as a person in this specialty, I still think women should do breast self-examinations. The reason they stopped recommending it is because, when they looked at the studies, the studies didn't show that it made a difference. Right, but I can tell you story after story of the woman that has come to me and has found her own breast cancer. Okay, so, yes, we're going to talk about how you should get your mammogram right, but I really want to emphasize how women have been their own advocate and they have saved their own lives by finding their cancer, because they felt something and they came in to see the doctor.
Dr. Michael Koren: 20:34
So interesting.
Dr. Sue Jane Grosso: 20:35
Yeah.
Dr. Michael Koren: 20:36
So your recommendations once a month, twice a month, uh, you know.
Dr. Sue Jane Grosso: 20:41
I would say it... I don't think you have to... I don't want to put that pressure on women and I think that's one of the reasons why they. You know, if a woman doesn't want to examine her breasts, I'm not going to push her and tell her that she has to. I think it's just, you know, becoming familiar, and you know I would say every so often, you know, maybe that would be every two or three months. You know, it's just, let's put it this way If you're in the shower, pay attention, see what your breasts feel like, and of course, some women will say, oh, but they're always, they feel lumpy.
Dr. Sue Jane Grosso: 21:11
I always feel something I can't tell, and I try to tell them. Believe me, when there's a cancer, it's going to feel different from anything else that you've ever felt in your breast, right? So, while I don't want to say that they have to examine their breasts every single month, that's not what I'm trying to say what I'm saying is, I think, being familiar with your breasts, how they when you, when you, look in the mirror, right?
Dr. Sue Jane Grosso: 21:36
looking in the mirror.
Dr. Sue Jane Grosso: 21:38
Is there a change with the way that your nipple looks? Is there a change with any of the color of at all of your, of your breasts? You see a dimpling, you know. Does one breast look different from the other? Size wise, I think it's important to to know what your breasts look like, believe it or not. Sometimes women have come in and I asked them. I said, well, how did you find this? And they'll say, well, my husband found it. I've heard that. I've heard where my dog kept going to this one part of my breast. You know, maybe because maybe the cancer was very warm, right, because of the extra blood flow or something. I've heard that story too. But you know, women should get their mammogram. I mean, let's start with that.
Dr. Michael Koren: 22:20
Just before we get off the breast exam, any advice vis-a-vis time of the month for women to examine their breasts, or doesn't matter that much?
Dr. Sue Jane Grosso: 22:26
I think that's a very good question.
Dr. Sue Jane Grosso: 22:28
And I think let's bring up the question about breast pain, right, because when you talk about time of the month, it's a woman who is menstruating okay can sometimes have tenderness of her breasts. Now, most pain is not associated with breast cancer, pain that is cyclical, meaning you can feel it before your period and then it goes away. You know, comes and it goes. That's not the kind of pain that is associated with breast cancer. And you're right as far as the best time to examine yourself will be, you know, after you had your period.
Dr. Sue Jane Grosso: 23:05
So let's say, at that, five or seven days, it's when your breasts become most quiet, as opposed to the middle or right before your period is when women, you know, are a little bit more tender, tend to be a little more full. So and in fact we don't do this so much anymore but when we do breast MRI and we'll talk about that at some other point we would try to schedule it at a certain point of their menstrual cycle, because the breasts are not as active. The breasts are very active, like right before your period. I think most women could probably, you know, probably would agree that that's when they feel it. So, yeah, I mean, but you know, to have to remember when to do it better, to just feel comfortable, to do it whenever, whenever you feel you want to. Yes.
Dr. Michael Koren: 23:49
So, moving on to mammography, I know you wanted to give some people some recommendations with regard to when that should be done and how frequently.
Dr. Sue Jane Grosso: 23:59
Well, you know, I think it's an important topic about when to start screening mammography and the reason why is because there has been a lot of controversy and there have been some differences among different organizations, and the differences tend to be the age group between 40 and 50, right Between 40 and 50,. It was not so long ago the United States Preventive Services Task Force. They had said that women between the ages of 40 and 50 did not require a mammogram and that is not what the American Cancer Society said and not what the American College of Radiology said. But recently they changed their minds and they have said that women from the ages 40 to 50 should get their mammogram. So if there's any woman out there listening anyone listening that's been a little bit confused with everything that has been said.
Dr. Sue Jane Grosso: 24:51
The bottom line is you start at 40. That is the age that you start. Now that's for women with an average risk. They don't have an increased risk, they are just average risk. Now some organizations, the same one I just mentioned, says that you should get a mammogram every two years, biennial, between the ages of 40 and 50. Actually they may actually say biennial from 40 all the way to 74. I have to check my records on that, but the American College of Radiology recommends that you do it every single year. So that is my recommendation. So does also the American College of Breast Surgeons say from 40 every single year. The American College of Obstetricians and Gynecologists also says the same. So age 40 every single year,
Dr. Michael Koren: 25:39
-a ny concerns about the radiation risk?
Dr. Michael Koren: 25:42
I know that's been thrown out there as a trade-off.
Dr. Sue Jane Grosso: 25:49
Right. Well, you know, look, with anything in medicine it's always about benefit and risk, right, you have to sort of look at what is the benefit, what is the risk. And with all of these guidelines, everything that we're talking about today, you should always talk to your physician, because your physician should be able to guide you oh sorry, there's a bug. Their physician should be able to guide you, they should know the information. If they don't know the information, they should call their radiologist. And I do get a lot of calls from my primary care, you know, colleagues, or you know gynecology colleagues that will call me to ask me what should I do? And that's what a patient should do is they should speak to their doctor.
Dr. Sue Jane Grosso: 26:23
Radiation, yes, there is radiation, but it's a low dose of radiation. And you can see, you know statistics out there that will tell you. You know, one mammogram is about 26 days of background radiation. And you know we're not talking about other parts of radiology, but CT scans of the abdomen and pelvis, for example, a lot more radiation than a mammogram. Chest x-ray is a little bit lower. So you have to sort of think about the benefit versus the harm. The radiation is very low and especially nowadays we have digital mammography and digital mammography is lower than film screen mammography, which is where we had started. So I could understand being concerned about radiation. I get it, but the benefit far outweighs any risk with radiation.
Dr. Michael Koren: 27:10
And that's helpful. So how about this concept of having the study done in the same place each year? So it's easier to compare. I'd love to hear your comments about that.
Dr. Sue Jane Grosso: 27:21
Yeah, that's a very good point. I'm glad you brought that up. It's very important for women to realize and know that we need to compare to priors, because sometimes the only way you can detect breast cancer is when there's a change in the appearance of the breast compared to before. So while I would tell you it is better to stay at the same facility so that they have the same you know all of your images from the past I don't want to say that you have to stay there, because what if you find another place that you prefer? What's most important is to get your prior mammograms and bring them with you to whatever facility if you choose a new facility right whatever facility.
Dr. Michael Koren: 28:11
-and there aren't compatibility issues with software and things like that, which is the bane of our existence in modern medicine.
Dr. Sue Jane Grosso: 28:15
Nowadays not. There were some issues when you had different machines because the vendors out there, the major vendors GE is one of them, Hologic those are probably the two biggest vendors. You have Siemens, you have other ones. At the place that I'm at, we have both GE and Hologic and they're very similar and there was a time when you couldn't upload the software from one mammogram to another, but that pretty much is non-existent nowadays.
Dr. Sue Jane Grosso: 28:44
Nowadays, if you and most places are digital I mean you don't film screen is not really something you see nowadays so much. Pretty much every place is digital nowadays. So you go to a place you can get your mammogram, put it onto a CD, and there are actually laws that protect women because the facility has to give them their images, and they actually there's a law out there that says you have to give it to them within like 15 days Like there are actually laws that exist to protect women. So, and at our place we have relationships with some other institutions where we can get electronic transfer of images as well. So I would say absolutely. I think that what's important is to know you need to compare to priors. That's the one important message that we have to give. At our facility we actually do get the patient to sign a release and then we will contact the other office and get them to mail it to us. So some places will do that for you.
Dr. Michael Koren: 29:44
That's terrific. So, moving on, you find something of concern on a mammogram and then you have to go to another form of imaging. So kind of walk us through what you do next typically CAT scan, ultrasound why you would pick the next modality based on what you're seeing.
Dr. Sue Jane Grosso: 30:01
Okay, good question also. So you start off with a screening mammogram. So at our place and most places, they are doing a digital mammography and they're doing what's called tomosynthesis, or it's also called 3D mammography, and that is a mammogram where the woman will experience that the machine moves as they're having their mammogram. That's because the machine is obtaining images right At different sections of the breast. It's kind of like a CAT scan, so it slices through the breast. It's like taking a loaf of bread and slicing that loaf of bread and imagine, you know, like the bread that has raisins, right, so you would be able to cut through and you'll find a raisin on the inside. So it's the same thing with a mammogram we get those slices. So if I'm reading a screening mammogram and a screening mammogram is someone that does not have any symptoms whatsoever If you have a lump, if you have any symptoms whatsoever, then you are not a screening anymore. Then you are what we call a diagnostic mammogram. A diagnostic mammogram means there's an issue, there's a problem, and you will come in and then your exam will be supervised, usually by a radiologist. Okay, so let's stick to screening. So if I'm sitting and I look at a screening mammogram and I see something abnormal, I'm going to call that patient back for additional imaging. So that's called a callback for additional imaging on another day. When they come back on another day, generally women will have additional mammography images and sometimes, and oftentimes I should say, they will also have an ultrasound. An ultrasound is different modality, it doesn't use radiation, it's ultrasound waves, but an ultrasound is very good at being able to detect a mass, a cyst. Sometimes we need to differentiate. Sometimes I look at a mammogram and I see a mass and I can't tell by the mammography because it just looks white. I can't tell if it's a solid mass or if it's a cyst, which is just a round collection of fluid, basically, which is completely benign and nothing to worry about. Once I get to evaluate the patient to see what they have and it could be calcifications, it could be a mass, it could be what we call architectural distortion, these are all things, that terminology that we use. Once we find that, then we have to decide whether that patient is normal and leaves and comes back in another year. Or does that patient maybe need to come back in six months, or is this patient ready for a biopsy?
Dr. Sue Jane Grosso: 32:36
Nowadays, for the most part, we do image-guided biopsies. It used to be years ago that women would go to the operating room for the surgeon to remove a piece of tissue, right the entire tissue, and that would lead to scarring, you know, disfigurement, sometimes potentially because you're taking. Now, most biopsies that we do are benign. They're not cancer. So the fact that we you know that what has been developed as image guided means that you could take a patient and just by placing a small needle into the area of abnormality, you could take a piece of the tissue right, a core, as we say rather than taking the whole thing out. Once that is done and that's usually done on a different day, right, usually not the same day as the callback the patient then has this biopsy. We find out what it is and if it's abnormal, the next step is the surgeon, right?
Dr. Michael Koren: 33:33
So the step that you described is prior to any surgeon getting involved. Do you have any sort of old school Staten Island and surgeons that think that that's not the best way to go out of curiosity, or is that pretty much accepted that there'll be a
Dr. Michael Koren: 33:47
radiologist that does the biopsy.
Dr. Sue Jane Grosso: 33:49
When I went back, when I went from California back to Staten Island back in 1993, at that time surgeons still believed that women should be going to the operating room it was very hard for them to accept that there was this thing called image-guided biopsies and that was part of what I had to teach them. But nowadays, years later, it has become accepted by everyone radiologists and surgeons that the first step in biopsy in a patient is image-guided biopsy. So the surgeons are completely on board with this because that is the standard. It's the standard for American College of Radiology and is the standard for American College of Surgeons that image-guided biopsy happens first.
Dr. Michael Koren: 34:35
So if a woman was recommended to have surgery first, they should be skeptical? Is what you're saying.
Dr. Sue Jane Grosso: 34:42
Yeah, and I don't know where that would be happening. But image-guided biopsies and I should say I think it's important to say, even though I'm a radiologist and I do image guided biopsies surgeons do image guided biopsies also. A surgeon may see a patient in the office and they may feel something right? A mass. And many of them are trained and they are accredited. Okay, they get certified to be able to do this and they, right there in the office, can put the anesthetic on the skin, go in, take a piece and send it off to the hospital.
Dr. Sue Jane Grosso: 35:13
So at our place at Summit.
Dr. Sue Jane Grosso: 35:14
Health, actually we have both. We have surgeons and radiologists. We both do the procedures, but I would say probably throughout the country, most places it's radiologists that are doing the biopsies got it all right.
Dr. Michael Koren: 35:27
So then next step. So hopefully it's benign. If it's benign, or you go back to the usual routine, or is that somebody at higher risk?
Dr. Michael Koren: 35:35
Uh, just, but based on the fact that I needed quote, a biopsy to determine what their status was.
Dr. Sue Jane Grosso: 35:41
Right if let's say let me just give an example this is a very common mass that we see out there, a fibroadenoma. So a fibroadenoma presents as a solid mass and sometimes you can tell that it's a fibroadenoma just by looking at it and you may follow it. But maybe you can't tell, so you do a biopsy. If I do a biopsy, then I have to do what's called assess the concordance. The pathologist tells me what it is right, they look under the microscope, they send me the report and then I look at my images and I look at the pathology and I say you know what this matches, we're good, she doesn't come back again until another year.
Dr. Sue Jane Grosso: 36:24
Okay, let's say I biopsy some calcifications and it comes back. That it's normal. However, maybe, for whatever reason I feel, I think I want to bring her back in six months so that I can do magnification views again, just to make sure that whatever piece I took was representative of the entire sample. Sometimes it comes back and there's something called atypia.
Dr. Michael Koren: 36:53
Mm-hmm.
Dr. Sue Jane Grosso: 36:54
So atypia. So there's atypical ductal hyperplasia, ADH, there's atypical lobular hyperplasia, ALH, and there's some other ones like flat epithelial atypia. So different types of pathology. If a woman comes back, the pathology comes back as atypical ductal hyperplasia. That patient does have to go on to the surgeon and that area then needs to be removed. And the reason why is because there have been cases. There are cases where the atypical ductal hyperplasia is just something that's telling you something's going on and they want to make sure there's no DCIS ductal carcinoma in situ, so that atypical ductal hyperplasia pathology does go on for more surgery.
Dr. Sue Jane Grosso: 37:40
The other atypias that I've said they don't. Now what if I do a biopsy and I feel that it's what we call discordant? Let's say it's an area that looks kind of suspicious. I do the biopsy and it comes back normal. But I say, yeah, you know, this doesn't seem right. Maybe my needle didn't go through to the right place, maybe it was a mistargeting of some sort, maybe the patient moved, maybe the anesthetic moved things, that patient. I may decide that that patient needs to go to the surgeon to have a larger area removed to be absolutely certain that there's nothing there.
Dr. Michael Koren: 38:18
Yeah, so again. So now we're getting into something that's more severe in terms of the diagnosis of cancer, and I know that you also use MRI technology and other types of technology. So where do they fit in and what's your part of sort of staging cancers in terms of spread and those type of concerns?
Dr. Sue Jane Grosso: 38:40
You know, for a cardiologist, Mike, you know a lot about this. You're asking all the right questions, for sure. Well, you know, look, sometimes when a patient comes in for a screening mammogram or when she comes back for additional imaging, sometimes I can look at it and I know that I'm looking at cancer. I mean, sometimes that does happen when you have a patient that has the possibility of cancer or you diagnose them as having cancer. The next step may be to get a breast MRI. So what is a breast MRI? That's magnetic resonance imaging. So breast MRI doesn't use radiation, it uses magnetic and radial waves. It's a completely different method or technology, but a breast MRI is very, very good at picking up invasive breast cancer. So while with a mammogram, especially when the breasts are dense, it may be difficult to see. So the patient may have cancer, but maybe I can't tell. How big is the cancer Like? How are we going to determine if she needs a lumpectomy or a mastectomy? You know, how do we know? So the radiologist can look at these images and say you know what? I think this patient would benefit from a breast MRI.
Dr. Sue Jane Grosso: 39:55
Now, if you look at what the American College of Radiology will say, they feel that every woman that is diagnosed with breast cancer should have an MRI. But some of our surgeons, some of our colleagues, do not believe in that, because there have been some studies and there haven't been studies that indicate that an MRI really does affect mortality. So not all patients that get a biopsy and diagnosed with breast cancer, not all of them, go on to breast MRI. Right Again, this is where you talk to your physicians, you talk to your radiologists and you get to find out what you need.
Dr. Sue Jane Grosso: 40:29
So now this breast MRI comes back to me again, and now I have to read the breast MRI and the breast MRI what it does is I get to see the breast that has the cancer, try to figure out how big it is, find out if there's any more disease right, because you could have one quadrant that has cancer but you may have cancer in another quadrant of the same breast. You get to look at the lymph nodes to see if there are any in the axilla or elsewhere. And the great thing is that you look at the other side, because about four to 5% of contralateral breast cancers may be there. So it gives you an opportunity. If the woman's going to go for surgery, you need to make sure that everything is okay right, not just one side, so that breast MRI is going to help to absolutely determine the extent of disease. Okay, now go ahead.
Dr. Michael Koren: 41:20
I was going to ask you.
Dr. Michael Koren: 41:21
PET scanning is another modality that people talk about.
Dr. Sue Jane Grosso: 41:24
I knew you were going to go there. So if a woman has breast cancer and it went to her lymph nodes, right, at that point the surgeon or the oncologist may say you know what I need to make sure, in order to stage this person, I need to make sure that there isn't breast cancer anywhere else, and that's where the PET-CT comes in. So PET-CT, that's positron emission tomography, right, and there is something called positron emission mammography as well. That's a little bit different. But the PET-CT which, by the way,
Dr. Sue Jane Grosso: 42:02
I did do a fellowship training in nuclear medicine as well when I was at NYU, and PET CT for me is one of my favorite favorite technologies, and that's because you look at the whole body all at once. The patient is injected with some radio tracer, right, it gets attached to glucose and it goes from your veins, it goes throughout your entire body and it gets picked up wherever there is a lot of uptake with glucose. So active cells, as you could imagine. The brain, right, our brain is very active. That brain lights up like you wouldn't believe. The heart lights up like crazy Certain things. The kidneys will light up everything but in the breast for the most part things are quiet right and things like the liver, the bones. So a PET CT scan is a great way to make sure that there isn't cancer anywhere else for that woman with breast cancer. So that definitely does help to stage her yes.
Dr. Michael Koren: 42:59
So interesting. So I have a couple other questions. Do you routinely look at genetic markers for breast cancer? Is that part of the history? When you're looking at the images, does that help you, does that hurt you? Just curious your perspective on how important that is. And if you're working in an integrated health system you may have that, but sometimes you may not have that. So maybe walk us through that, whether or not you recommend those things for women that may be at high historical risk.
Dr. Sue Jane Grosso: 43:28
Okay, well, you know one of the things that when a woman comes in to get a mammogram, we do obtain a history. We have a history sheet that they fill out, and part of that history sheet is to find out number one does she have a complaint? We need to know if she has a lump or if she has what we call focal pain. Right, we find out about family history. Who else in your family has breast cancer? At what age did they develop breast cancer? Does anybody else have ovarian cancer? And same thing is have you ever had a biopsy before? Have you, and is there any genetic mutation that we should know about? So all of that is extremely important. And as you bring that up, I should also bring up something that's called risk assessment, because a lot of breast imaging facilities have this. They have programs that assess your risk for the development of breast cancer over your lifetime.
Dr. Sue Jane Grosso: 44:27
So one of the ones that we like is called Tyrer-C uzick, and I can get into that a little bit more later, but you're absolutely right that when a patient walks in, all of her history is very important, so that it helps me figure out what I need to do next.
Dr. Sue Jane Grosso: 44:43
It's not going to change how I read her mammogram, because I'm there to read the mammogram and find out is there something abnormal? But if I find out that the woman has this history and, let's say, her breasts are extremely dense, right, and we haven't gotten into density yet, but density is one of the things that affects the ability to see tumors on a mammogram. So if that woman has significant history and she has very dense breasts, I may recommend that she have a breast MRI, right, or I may recommend that she have an ultrasound, or I may recommend you know what. You need to see a breast specialist, because you also need to see a geneticist to find out about your markers, right, so that patient is going to get plugged in, possibly into a high risk program, for example. So you're right Knowing genetic mutations? Absolutely. Now, remember, most women with breast cancer do not have any genetics or any family history. 85% of all breast cancers have nothing to do with family history or genetics.
Dr. Michael Koren: 45:48
Interesting.
Transcript Generated by AI.
Announcer: 0:00
Welcome to MedEvidence, where we help you navigate the truth behind medical research with unbiased, evidence-proven facts Hosted by cardiologist and top medical researcher, Dr Michael Koren.
Dr. Michael Koren: 0:11
Hello, I'm Dr. Michael Koren, the executive editor of MedEvidence! And I've been having a fascinating discussion with my colleague from medical school, Sue Jane Grosso-Rivas, and we've been talking about many issues related to breast imaging. This has really been a masterclass and I want to thank Sue Jane again for being part of it. You mentioned the breast density. Does that change the basic recommendations of yearly mammographies or do you go straight to other imaging forms for those type of folks?
Dr. Sue Jane Grosso-Rivas: 0:40
Yeah, no. What has happened in the past few years is that density has become something that everybody is talking about, right? First it was get your mammogram, get your mammogram. And then it was, oh, get your mammogram. But you also need to know if you have dense breasts, to the point where now there are laws,
Dr. Sue Jane Grosso-Rivas: 1:09
There are federal laws that exist that say that you must notify patients about this thing called density. What do you communicate? You have to communicate in there because we send lay letters. We send the report to the patient, but they also get something that's called a lay letter and in that letter there is actually a phrase or two that is mandated by the government that says you may have dense breasts. This is what happens with dense breasts. Dense breasts may obscure, so there's a whole phrase that goes into that. So women now need to be notified about this thing called dense breast. And why is that? Because, yes, dense breast can obscure, sometimes a tumor.
Dr. Sue Jane Grosso-Rivas: 1:50
You know, mammography is pretty good at detecting breast cancer, but when you start going into the dense categories it starts to lower the sensitivity of mammography for breast cancer. So some of those patients may require supplemental screening and we should start with ultrasound first. Right, because ultrasound is another modality and it's been shown that if you do mammography and you add ultrasound, you will pick up some more cancers that you did not pick up by mammography. The next step would be do you have to go to MRI? Right, because MRI is going to. But if a woman has average risk, should you be, should you recommend MRI?
Dr. Sue Jane Grosso-Rivas: 2:32
MRI is really more for the patient that is either diagnosed with breast cancer or has an increased risk. Most of the women with average risk. You can stop after the ultrasound. Right, you're done. You've done everything you need to do. But as a radiologist, I still maintain the ability to decide what I think that patient needs. So I may look at a mammogram and I may describe what I would call a complex parenchymal pattern, and what I mean by that is that when I look at her breasts, not only is she dense, but I see nodules here, nodules there, like masses, or I see lines. I just see that she's very complex and I know that I feel that that patient really needs to go to MRI next. So the radiologist always maintains the ability to be able to say what needs to be done next.
Dr. Michael Koren: 3:27
Approximately what percentage of women have this dense breast phenomenon?
Dr. Sue Jane Grosso-Rivas: 3:32
Well, according to what you know, the lexicon, meaning the American College of Radiology, and they've done a lot of studies about 40% of the population, oh wow. So there are four categories. It's A, B, C, D. A is completely fatty. B is what we call scattered fibroglandular, which is just 25% of this tissue. Right, that becomes kind of white. C and D are heterogeneously dense, which is 75% of the tissue is there and extremely dense is. You know, almost all of it is white. So when they look at this, they say 40% of women have dense breasts. They're in the category C or D.
Dr. Sue Jane Grosso-Rivas: 4:16
Now I will tell you that certain communities have more dense breasts than other communities. So if you go to certain parts of the country, right, it could be body habitus, some women, you know, when there is some obesity, right, those women tend to have more fatty breasts. And when you have women, you know, maybe in a population where everybody's exercising, they're on hormonal replacement therapy, you know, they're very thin, they watch their weight those women are not going to have as much fat in their breasts. Now, density is determined by genetics. You're either dense or you're not dense. But it also is affected by whether you have hormones, whether you exercise all the time there's no fat, so on and so forth. But it was funny because when I went from Staten Island and came to where I work now, it was complete. I could not believe how many women were dense. So I would say it's not 40%. In my neighborhood, in my community where I am now, I would say 60 to 70% of women are dense.
Dr. Michael Koren: 5:19
Really, and that's in New. Jersey right
Dr. Sue Jane Grosso-Rivas: 5:21
Yeah New Jersey.
Dr. Sue Jane Grosso-Rivas: 5:22
When, of course, sometimes you may have heard New Jersey supposedly has a higher incidence of breast cancer, because that's the other thing. It's like going to different parts of the country you find different incidence of breast cancer and the population in New Jersey is very large; a lot of breast imaging centers in New Jersey.
Dr. Michael Koren: 5:42
And the epidemiology of breast cancer when I was doing internal medicine was that if you had your first child later in life, you're more likely to get breast cancer. Is that still considered to be accurate?
Dr. Sue Jane Grosso-Rivas: 5:52
Yes, they still use that and this risk assessment that I told you about. That's some of the questions that they ask. They will say have you had children? When did you have your first child? Right, so if you had your child younger although they say like less than 20 is is most protective, I mean most women are not going to have it at that time. But, um, so what? Also, when did you have your menstruation, your first menstruation? It's like the earlier you had the menstruation, the more risk. Uh, when did you have menopause? The later you have menopause, the more risk. So those questions are all asked in the risk assessment. So that's still all part of it, but the single most important thing is just being a woman and getting older.
Dr. Sue Jane Grosso-Rivas: 6:36
I mean that's why you need to get checked out.
Dr. Michael Koren: 6:40
So this is fascinating. I'm loving all this information. Thank you for sharing it. So there's two more things on my mind that I want to cover. One is AI that's what everybody talks about, and the other one is men. We'll make that last, but hopefully not least. So, lets jump into AI, and certainly AI is the buzzword, and it has affected different areas of medicine.
Dr. Michael Koren: 7:03
I like to tell my staff here that for every incidence of AI I see an incidence of AS artificial stupidity, and I don't know if you want to comment, but we've heard that it is having a big effect in imaging overall and maybe particularly breast imaging. So tell us a little bit about what's happening with AI.
Dr. Sue Jane Grosso-Rivas: 7:22
Sure, you know, Mike. What's interesting is I met with a colleague the other day and her son happens to be in medical school right now and she's a radiologist. So she thought that radiology would be a wonderful field for her son and her son said no, mom, AI is taking over, I'm not going to go into radiology, I won't have a job.
Dr. Sue Jane Grosso-Rivas: 7:46
So very interesting for me to hear that that is what they are possibly hearing right At that stage of medical school where it's affecting whether people go into radiology or not, because they're so concerned that AI is going to take over. So artificial intelligence, right, what is it doing? Well, look, is it good. There's good and there's bad, always right. So with AI and we had something before AI we had something called CAD, which was computerized assisted diagnosis, right, or computerized assisted detection, and we now have CAD. We've had CAD for years, years, and what the CAD does is it helps to point out, for example, where there are calcifications, because calcifications may be the sign of early cancer, ductal carcinoma in situ it's only in the ducts hasn't invaded. So, as a radiologist, one of the things we look for is calcifications, but sometimes they're very tiny, they're very difficult to see. So the software will pick up where there are calcifications and it puts a mark around it and it says look here, look here. And that saves you sometimes, right, because the radiologist somehow didn't see it because it was so tiny. So we've had that for a while, because it also even picks up masses or distortion. But now AI is around and there are quite a few radiology practices that have it already.
Dr. Sue Jane Grosso-Rivas: 9:09
So I just want to talk about the breast imaging part. So tomosynthesis right, that's the one I told you about that slices through the breast and there are several images. Now one breast could have 80 something images. Like we don't realize. We went from four images of the breasts to now having, you know, 80 images of one breast, 80 images of the other breast. I mean it gets to be almost too much all the slices that you have to look at.
Dr. Sue Jane Grosso-Rivas: 9:38
So AI for us, what it does, it's got an algorithm that has been developed over time. Right, these companies make them better and better with time because they feed them with information of you know, this is what a cancer looks like. You feed them all this information and now this algorithm comes along, looks at the images, those 3D images, and it says here it is, there's a cancer right there. There's a cancer right there. Look here, look here, look here. And there have been some studies that are saying that AI is picking up some cancers that the human eye has not picked up.
Dr. Sue Jane Grosso-Rivas: 10:14
Right, we're only human. Sure, you know we're we could possibly not see a subtle finding. Do I think AI has replaced the radiologist? Not yet, not not at this point. I have AI for one of the offices and what'll happen is it'll point to something for me, but ultimately it is the radiologist that has to look at those images and evaluate it and decide is AI being stupid right now or is it really something? And then you decide whether that patient has to come back or not. So I think we need to learn how to live with AI in our world. Basically.
Dr. Sue Jane Grosso-Rivas: 10:53
Right.
Dr. Michael Koren: 10:53
So we're certainly not at a point where a radiologist or a group or a process that doesn't use AI is somehow behind the times. Right, we're not at that point.
Dr. Sue Jane Grosso-Rivas: 11:04
You have to be with the times, for sure, and you have to learn. You know, with every new technology that comes along and we haven't even talked about contrast enhanced mammography, which you probably probably should mention, but with every technology that comes along, you have to kind of embrace it, you have to look at it and you have to see, well, how does this help me? You know, how can I use this to make me a better physician? What can this do for me? And that's kind of the way that I'm looking at it. I'm towards the end of my career, so I'm not worried that AI is going to replace me.
Dr. Michael Koren: 11:35
I think, based on the way you look, you're at most halfway through.
Dr. Sue Jane Grosso-Rivas: 11:39
Yeah, Okay, Okay, Mike, let's just say that that's true. But I mean, I enjoy what I do, so I'm not going anywhere anytime soon. But yeah, no, AI is here and and you know it's. It's going to be interesting to see what happens in the future with AI, because it's also going to be used for magnetic resonance imaging. It's being used in many different areas of radiology at this point, so it remains to be seen.
Dr. Michael Koren: 12:00
So you mentioned contrast imaging, so go ahead and give us the quick spiel on that.
Dr. Sue Jane Grosso-Rivas: 12:05
Okay, so we talked about x-rays being static, but you know, contrast enhanced mammography and MRI with contrast is not static, it's more functional, it's more physiologic. You know, with contrast agents, if you put either iodinated contrast IV for contrast enhanced mammography, it's the same IV contrast that they use for CT scans. Or if you use a radio tracer, like for positron emission tomography, all of these types of studies, the agent goes into the body and it goes to a particular place where for positron emission tomography, it's where they're using glucose.
Dr. Sue Jane Grosso-Rivas: 12:44
With contrast enhanced mammography and magnetic resonance imaging it's about flow. Cancers develop blood vessels. That's what cancer does. Cancer wants to grow, so the vessels are created and it grows. And guess what? The blood flow goes to that cancer and then it shows up. So contrast enhanced mammography means I'm doing a mammogram but I'm giving you some contrast because I want to see the flow. I don't know, I don't want to see white. They're subtraction images and it's going to show me where there is a lot of blood flow. And where there is a lot of blood flow is where there's going to be a cancer, and that's the same thing with magnetic resonance imaging. Contrast enhanced mammography's going to be a cancer. And that's the same thing with magnetic resonance imaging Contrast enhanced mammography is going to take off.
Dr. Sue Jane Grosso-Rivas: 13:32
That's one of the newest technologies and they have a study going on right now. It's called the CMIST trial. It's basically GE, together with, you know, actually Estee Lauder company. I forgot the name of it. I think it's called Breast Cancer Research Group, I think it's called. So they've come together and they are looking to see if women with dense breasts, with average risk, will benefit from contrast enhanced mammography. And that comes up and shows us that it is a good study. I think we're going to see a lot more of that for sure.
Dr. Michael Koren: 14:08
Wow, fascinating.
Dr. Sue Jane Grosso-Rivas: 14:09
Because, it's easier. Contrast-enhanced mammography takes about anywhere from five to eight minutes, whereas magnetic resonance imaging takes more like 30 minutes 35 minutes. And MRI is very expensive. Contrast-enhanced mammography isn't. So there are a lot of pros basically for contrast enhanced mammography. But having said that, nothing beats breast MRI. Breast MRI is still at the top as far as being able to show invasive breast cancer. Abbreviated breast MRI is one of the newer technologies where they've learned that they don't have to do the study for as long. They just have to do one or two images and they get to see what they need to see. So it's much shorter scan time.
Dr. Michael Koren: 14:53
Interesting.
Dr. Michael Koren: 14:54
So, last but not least, men and breast imaging
Dr. Sue Jane Grosso-Rivas: 14:57
oh men, yes, yes, and I do get to see a few men in my practice.
Dr. Michael Koren: 15:01
The forgotten sex, go for it.
Dr. Sue Jane Grosso-Rivas: 15:05
Yes, well, for the men, only 1% of all breast cancers are in men, you know, whereas women, the number of invasive breast cancers that may be shown this year maybe, you know, greater than 300,000,. Let's say a man, the men will have breast cancer, maybe 2000, you know of all the breast cancers. So it's not common. It happens as they get older. So most of the breast cancers you see in men are over the age of 60. Men do not get screening mammography. Okay, that hasn't been instituted. The way that men present is that a man will feel a lump. When they feel a lump on clinical, or if the doctor feels a clinical on clinical exam, they feel a lump. That's when they end up coming to me. I will do a mammogram on a man. Okay, they have enough breast tissue to be able to do a mammogram and we're looking for cancer. Generally. The difference, you know, or what we're looking for basically in men, is they feel a lump. Is the lump cancer or is it something benign, like gynecomastia, which is the development of breast tissue which does happen with a lot of men as they get older. Also, many men that have prostate issues. They're on certain medication that affects the breast tissue, they start to develop breast tissue, just like women. Okay, so that's usually what I'm trying to evaluate. And you know, sometimes doctors will send the man for an ultrasound, but the ultrasound is not what we need. We need the mammogram. You have a lump, you get mammography.
Dr. Sue Jane Grosso-Rivas: 16:41
Now what if a man has a genetic mutation? Because this is the other thing. People used to think that your mother's history was the only history that was important. That's not true. Now we want to know your family history on your mother's side and your father's side, because your father could have the mutation.
Dr. Michael Koren: 17:00
Yeah, makes sense.
Dr. Sue Jane Grosso-Rivas: 17:01
If the father has the genetic mutation, then that's going to increase his risk for breast cancer, as well as his children. So, yes, and men don't get screened, but men do well If their breast cancer is identified. They usually get identified early because men don't have a lot of breast tissue, so it's very easy to feel you know the cancer basically. So men do tend to do well.
Dr. Michael Koren: 17:28
Yeah, In the cardiology world we use a drug called spironolactone quite a bit that causes gynecomastia and if we identify that, is that a reason to get a mammogram or just get them off the spironolactone?
Dr. Sue Jane Grosso-Rivas: 17:41
What ends up happening is that they, you know it doesn't feel comfortable for a man when they start, you know, because what happens is they develop breast tissue and they'll develop tenderness, which is uncomfortable. So sometimes what ends up is you'll have to get them on something else, some other medication, basically you know,
Dr. Michael Koren: 17:58
But they don't necessarily need to be imaged, I guess, is my question.
Dr. Sue Jane Grosso-Rivas: 18:06
He has to be imaged.
Dr. Michael Koren: 18:07
he has to be Okay. Oh, interesting,
Dr. Sue Jane Grosso-Rivas: 18:08
If you, if you feel a lump and he's on spironolactone, there's no way to know if the lump is because of the spirono lactone, with gynecomastia, or is there cancer.
Dr. Michael Koren: 18:13
Or if there's no lump, just enlargement of the breast. Do you still recommend a mammogram?
Dr. Sue Jane Grosso-Rivas: 18:17
I would still do imaging. I would do imaging, yeah.
Dr. Michael Koren: 18:20
Yeah, well, I'm going to be sending you some referrals then in the near future, all right, that sounds good.
Dr. Sue Jane Grosso-Rivas: 18:25
So you know
Dr. Sue Jane Grosso-Rivas: 18:26
one thing I do want to mention, because you're a cardiologist what about arterial calcifications on a mammogram? Have you heard about that?
Dr. Michael Koren: 18:35
I've heard of them. I'm not sure exactly what I would do, but I do get a lot of referrals from other imaging to cardiology because of concerns about coronary calcium. But go ahead. I'm sure you see that as well, yeah.
Dr. Sue Jane Grosso-Rivas: 18:48
I mean it's very interesting because when I look at a mammogram and I'm looking for calcifications, sometimes I see vascular calcifications, so breast arterial calcifications. Now, let's say it's a woman, that she's in her 40s and I see a lot of calcifications in her. You know vessels. I do report it. Not all radiologists necessarily report it, but we all know that there does seem to be some association with, uh, having vascular calcification seen in your breast. There seems to be some association with cardiac disease and also the potential for developing a stroke. So you know, as a woman gets older, you'll see vascular calcifications more right, because basically she's developing calcifications everywhere, which includes the breast. So it is something to mention and maybe it's an opportunity for the primary care physician to sort of look at that patient and start assessing. You know, how is this person's cardiac health? Because ultimately we're talking about breast cancer, right? But the leading cause of death in women is still cardiac disease right.
Dr. Michael Koren: 19:52
So A lot of women forget that, unfortunately.
Dr. Sue Jane Grosso-Rivas: 19:54
Yeah, no, it's like, you know, breast cancer. And breast cancer is not even the leading cause of death. It's lung cancer still, but breast cancer is still the leading cancer. We should say but so, yeah, so if there are arterial calcifications of the mammogram, we shouldn't totally ignore them, because that may help to determine if she has some cardiac disease.
Dr. Michael Koren: 20:17
And I'm going to throw my final question out at you a little bit out of left field, but it's something we've addressed here in MedEvidence.
Dr. Michael Koren: 20:35
What are your thoughts about alcohol and breast cancer risk?
Dr. Sue Jane Grosso-Rivas: 20:37
Well, I think, like with anything, as far as risk is concerned they always askhow can I , " "Reduce my risk of breast cancer, right? So you're going to hear from any doctor for any cancer, right? Lifestyle you know. Obesity they say with obesity there's an increased risk. You know. You want to eat well, you want to exercise, you know all of these things. But then yet I can tell you about my very good friend who was at the age of 40. She was a runner, right. She drank, you know, green juice or whatever it is she was doing. She had cancer, right. So it doesn't just because you do all these things doesn't necessarily protect you. Alcohol, from what I've heard and actually I was listening to one of your podcasts, I think from Med Evidence, and I did hear you guys talk about alcohol, but everything in moderation is the way I feel. I feel to say to someone don't drink alcohol at all.
Dr. Sue Jane Grosso-Rivas: 21:30
I don't think that makes any sense, Just like, you know, don't drink coffee, right? If a patient comes into me, she's got multiple cysts. We know caffeine can affect the breasts and they could end up developing more cysts. But are you going to tell someone, well, you've got to stop caffeine. You know completely. Very hard to do, I think if someone's drinking alcohol on a daily basis, that's too much and I do think that that is of concern. So, yeah, no, I would say.
Dr. Michael Koren: 21:57
All good things in moderation is the lesson.
Dr. Sue Jane Grosso-Rivas: 22:02
I personally think, all good things in moderation, but we still don't know exactly what's causing the breast cancer. Right, I already told you that most of it is not genetic that we know of, although every year, right, every time, we hear about more genes, more genes, and I, for example, we haven't really talked about stories. I have so many stories of patients, but a friend of mine, his daughter, just passed away at the age of 34 from metastatic breast cancer and there's nobody in the family, just nobody in the family. So why, you know those, those cases that I know of where there's no? And then I have another person who's uh, was a technologist of mine, you know developed DCIS at a young age and no genetics, nothing. And then her daughter, at the age of 31, finds her own, feels her own breast cancer, okay, saves herself, basically. No genetics! So so what's going on, so you know, and and we didn't get into is that we are finding we didn't talk about black women and there's a big problem that's going on. And the ACR has now actually issued some new recommendations and this is very important to say right now which is that all women should have their risk assessment at the age of 25 to 30.
Dr. Sue Jane Grosso-Rivas: 23:21
And what that means is that when you go in to see your, you should go in to see your primary care physician, because a lot of women don't know that there is this genetic predisposition. We need to know if there is family history. You know how many times I talk to a patient and they don't even know their history and when they find out there's something abnormal, they go back and start talking to all their family members and then they find out oh yes, aunt so-and-so, cousin so-and-so. They start finding out all of these histories. Well, that's what the new recommendation by the American College of Radiology you got to find out by the age of 25 to 30. And why? Because if there is a genetic predisposition or significant family history, that woman may need to start earlier than 40 to get her mammogram. That woman may need to get breast MRI, for example.
Dr. Sue Jane Grosso-Rivas: 24:11
Right, and what they found is that something is happening within the black women, the ages of some of them, because you can get cancer between the ages of 20 and 29. It's not common but you can, and what they found was that black women are getting the 50% more cancers in in black women from the ages of 20 to 29 than their white women counterparts Right 30 to 39, it's only about maybe 17% increase. Something is happening and many of the black women get the more aggressive type of breast cancer. It's called triple negative, meaning it's ER negative, pr negative. You know, estrogen, progesterone negative and HER2, herceptin negative. They are much more aggressive cancers. So you know, it's almost you know, a warning that's going out there to let everybody know.
Dr. Sue Jane Grosso-Rivas: 25:01
Hey-
Dr. Michael Koren: 25:01
Any theories as to why that is? Out of curiosity?
Dr. Sue Jane Grosso-Rivas: 25:04
They're looking into the possibility. They want to look at the type of cancers, the molecular basis, but what they have found overall not even just black women, asian women, right, they have a lower incidence in general, but they're finding that the younger women are starting to have more, there's more of an incidence of breast cancer, and people are trying to figure it out. And a lot of these breast cancers are estrogen receptor positive and progesterone positive also, so they tend to be estrogen type tumors, right? So I don't know, we haven't figured out exactly what is going on. But then let's go back to lifestyle. That's what I'm saying. So what is it?
Dr. Sue Jane Grosso-Rivas: 25:45
So, if you ask me about alcohol, you know, is it related to the way you're living your life, right? Is it related to the way that you're eating? Is it nutrition? Is it the environment? What do we have in our environment? The microplastics? I don't know right. There's got to be. There's something that's happening. The good news is that for the past 50 years, the mortality rate for breast cancer has dropped significantly. So there is no doubt that we are doing a better job with all of the screening, mammography, maybe the new chemotherapies that are out there. Whatever it is that we're doing, it is much better. Women are surviving breast cancer. There's no doubt about it that they are. Whether it's stage zero, stage one, stage two, women can still survive their breast cancers, absolutely so that's the good news.
Dr. Michael Koren: 26:39
So, Sue Jane, a lot of people are concerned about the cost of health care. Tell us a little bit about what the expectation should be of a woman who needs these screening procedures and what her insurance company should pick up and what the cost should be approximately.
Dr. Sue Jane Grosso-Rivas: 26:54
Well, you know, at this point, because all of these organizations have agreed that screening mammography should occur, right, they should be able. Their insurance company should be paying for their screening mammography.
Dr. Michael Koren: 27:08
Zero out of pocket usually?
Dr. Sue Jane Grosso-Rivas: 27:10
Usually a zero out of pocket, usually. Now they may have, however, a deductible that they have to meet, right? So I shouldn't say everybody, everyone's insurance is different. Let's talk about Medicare, for example, right, medicare. Like most women that come for their mammograms, many of them are older, they're Medicare age. So the woman must know what the Medicare rules are, because you know if they come just a few days too early, you know if it has to be exactly at 12 months that they can get their mammogram. If not, then they will be responsible for the bill, right? So they need to be aware. Some insurance companies will say you don't have to wait a whole year, just do it at some point in the year. So it just has to be, you know, this year, next year, it doesn't matter what month. Every woman has to be aware.
Dr. Sue Jane Grosso-Rivas: 28:00
Now there are screening programs out there. You know that that will pay for free mammographies. And you know in in New Jersey there's something called the seed program and that seed program will help women get mammograms for free. So there are ways of getting free mammography. But as far as insurance is concerned, yes, you're right, this is something you need to look into because if that insurance company believes that you should only get mammography every two years. They may not pay for every year, right. But what about supplementary screening? Your radiologist reads it and says you need an ultrasound and your insurance company turns around and says, no, you don't, right, that's a problem. So you need to know what state you live in and you need to know what the laws are, because there are states where the law does protect you and the insurance company has to pay for your supplementary study. The only way to know is to speak to your insurance company. Many women go back and fight with their insurance companies if they have to.
Dr. Sue Jane Grosso-Rivas: 29:02
Breast MRI is another issue. Sometimes you hear breast MRI. Well, we can't get the insurance company to agree to do the breast MRI. So I'm very careful in my reports. I make sure that I make it very clear as to why I am recommending this breast MRI, because that report is going to help determine whether her insurance company will pay for it. But you're right, you have to.
Dr. Sue Jane Grosso-Rivas: 29:24
And how about this? When should you stop doing a mammogram? And I'm sorry we didn't get to talk about this, but this is important because many organizations will say stop at 74. I mean 74-year-olds say, 75, I mean nowadays people are living much longer, right? So the American College of Radiology says this, and I believe this as well you stop when you are no longer going to be in good health. If you're going to be in good health for the next 10 years, then you should continue to get your mammogram. So if you got a 74-year-old and she's doing very well and she expects you know, the doctor feels like she's probably going to live until 84, then yeah, she should continue getting her mammogram, right. So, but what if the insurance company doesn't pay for it? That's a problem.
Dr. Michael Koren: 30:18
Well on that. I truly want to thank you for the MedEvidence family for a true tour de force. Thank you, Sue Jane, for a true masterclass on breast imaging. I learned a tremendous amount. I'm sure our audience will share that sentiment quite a bit. And thank you for sharing your story about Ms. Goldberg. And thank you for just a tremendous number of very pragmatic insights that I'm sure will make a difference in people's lives.
Dr. Sue Jane Grosso-Rivas: 30:48
My pleasure. My pleasure Any opportunity I have to get information out there. I just think it's what I'm here to do.
Announcer: 30:56
Thanks for joining the MedEvidence podcast. To learn more, head over to MedEvidence. com or subscribe to our podcast on your favorite podcast platform.